Published: Jan 17, 2014
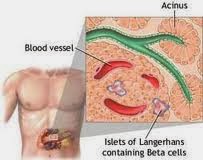
The new approach involves silencing a region of chromosome 11 (CDKN1C), where the cell cycle inhibitor p57Kip2 resides. Loss of beta cell mass, which results in decreased insulin production, is one of the exacerbating factors in type 2 diabetes.
The researchers suppressed CDKN1C expression in human islets taken from deceased organ donors and transplanted them into hyperglycemic, immune-deficient mice. Beta cell replication increased more than threefold, Klaus H. Kaestner, MD, of the University of Pennsylvania in Philadelphia, and his co-authors wrote online in the Journal of Clinical Investigation.
"The newly replicated cells retained properties of mature beta cells, including the expression of beta cell markers such as insulin, PDX1, and NKX6.1," the authors wrote. "Importantly," they added, "these newly replicated cells demonstrated normal glucose-induced calcium influx, further indicating beta cell functionality."
The stimulatory effect of p57Kip2 suppression is particularly "remarkable," the authors wrote, "considering that these studies were performed on islets from deceased organ donors over the age of 50 years, an age when significant beta cell proliferation was thought to be impossible."
Suppression of p57Kip2 did not result in "appreciable" DNA damage, in contrast to previous research in which beta cell replication was encouraged using forced expression of cell cycle regulators, the authors wrote. "Thus p57Kip2 is a promising target for diabetes therapy via beta cell mass expansion," they said.
The approach outlined in this research was suggested by the observation that, in children born with focal hyperinsulinism, silencing of p57Kip2 results in "dramatic, non-neoplastic clonal expression" of beta cells.
"Previous studies have shown that beta cells can be pushed to replicate, so this is not the first observation of that. But the fact that they were able to show this does not cause damage is pretty compelling," Rohit N. Kulkarni, MD, PhD, of the Joslin Diabetes Center in Boston, said in an interview.
A key next step, said Kulkarni, would be to demonstrate control of the cells once they're activated. "Although this protein has been shown to be critical for that replication process, being able to safely replicate it so that you can control the replication and switch it on and off would be important."
Kulkarni also said it was useful that this was done using a human mutation, rather than a mouse model.
Because p57Kip2 is not expressed in rodents, the researchers used islets from deceased human organ donors. "Transduction of human islets with p57Kip2 shRNA lentivirus caused over a 70% reduction in CDKN1C mRNA levels in infected cells," the authors wrote.
Attempts to stimulate beta cell replication in vitro were unsuccessful. "Therefore, we chose to transplant transduced human islets under the kidney capsule of immunodeficient mice, which allows for islet revascularization and exposure to host factors," said the authors.
The results of this study, the authors wrote, do not exclude the possibility that other genes in the imprinted region of chromosome 11 may contribute to clonal beta cell expansion in focal hyperinsulinism. If other genes exist, they too could be targeted to enhance beta cell replication in adult cells, the authors said.
Source: http://www.medpagetoday.com/Endocrinology/Diabetes/43857


0 comments:
Post a Comment